by Paul Fassa
Health Impact News
A new study published in the journal Plant Foods for Human Nutrition on August 31, 2018, with the title Beneficial Effect of Virgin Coconut Oil on Alloxan-Induced Diabetes and Microbiota Composition in Rats adds further proof that virgin coconut oil is a powerful remedy for diabetes.
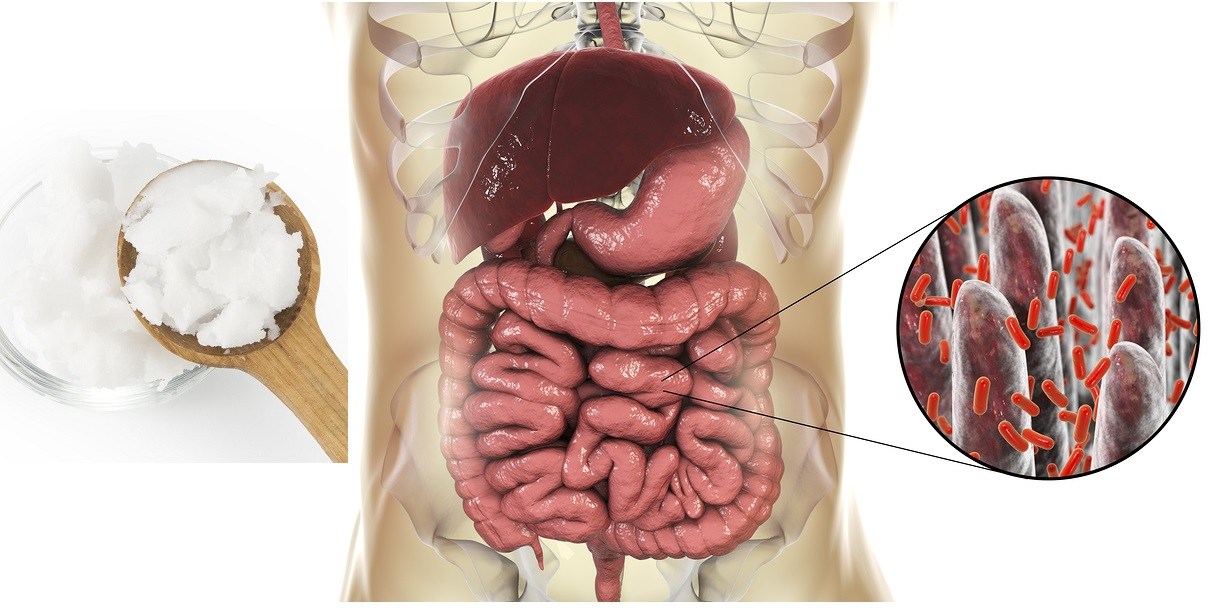
In this latest study, virgin coconut oil was shown to be beneficial to the microbiome by increasing probiotic bacteria, leading to better outcomes for those suffering with diabetes.
This new research confirms what many have reported to us over the past 15 plus years, that virgin coconut oil is beneficial in overcoming both Type 1 and Type 2 diabetes. See:
Coconut Oil Effective in Treating Diabetes
This new study offers a possible explanation as to how virgin coconut oil helps people with Type 1 diabetes without directly affecting insulin levels.
The Study and Its Findings
Researchers at the University of Belgrade in the Republic of Serbia gathered 24 Male Wister rats around 2.5 months old caged in pairs. All were fed standard commercial feed and tap water without rationing.
According to Fluoride Alert, only three percent of Serbia’s tap water is fluoridated. Regardless of the Belgrade lab’s tap water purity, the rats all drank the same tap water during the 16-week study.
The four experimental groups of six rats were categorized according to their dietary intake:
- Control group (Con) with its diet of rat feed and tap water only.
- Virgin Coconut Oil (VCO).
- Alloxan (Alx) to induce diabetes in the rats.
- Alloxan plus Virgin Coconut Oil (Alx + VCO) group.
A small amount of saline water was subcutaneously administered to the rats on the first day only to “allow comparability with the other experimental groups”. The rats’ body mass, food, and water consumption were monitored continuously during the whole 16-week experiment.
Their blood glucose (glycemia) levels were measured after a 16-hour fasting period at the end of each week during the 16-week study.
Stool samples were taken from each pair of caged rats and frozen at minus 80 degrees C (Celsius) or minus 112 degrees F (Fahrenheit) and saved for stool bacterial analysis.
The alloxan was administered by intraperitoneal injection (I.P.), which is an injection into the abdominal cavity of the rats at a standard amount of 150 mg per kg of weight as used in other studies that induced type 1 or insulin-dependent diabetes, as noted in section 2 of this source. This distinction is discussed in the commentary below.
This study’s conclusion as extracted from its abstract:
Although the intake of virgin coconut oil did not decrease the diabetes-induced hyperglycemia, it affected the secondary parameters, such as food and water intake and average body mass gain.
Furthermore, its potential to positively affect the fecal microbiome was proved, since it significantly increased the abundance of probiotic bacteria, such as Lactobacillus, Allobaculum, and Bifidobacterium species.
The takeaway from this study is in the increased microbiome probiotic content from VCO (virgin coconut oil). From the study text:
Our results proved the potential of virgin coconut oil to positively affect the fecal microbiome, with a significant increase in the abundance of probiotic bacteria, such as Lactobacillus, Allobaculum and Bifidobacterium species.
Study Commentary
The fact that there was no significant positive hyperglycemia (high blood sugar) reduction is due to the nature of what Alloxan induces – Type 1 diabetes. With this form of diabetes, the pancreas beta cells that normally produce insulin are challenged in some way that inhibits or prohibits insulin production.
Thus, there is not enough insulin produced to usher glucose into cells for metabolic conversion into cellular energy, forcing insulin dependency with self-administered injections or insulin pumps attached to diabetics’ bodies.
Type 2 diabetes is the result of poor lifestyle and dietary habits that lead to metabolic syndrome or insulin resistance syndrome, and then type 2 diabetes. At no point should there be any insulin dependence among type 2 diabetics, because their hyperglycemia issue is not with a diminished pancreatic production of insulin.
Type 2 diabetics have enough, and sometimes more than enough, pancreatic insulin production. But the cells that need to metabolize glucose with oxygen and produce energy aren’t able to pack-in the insulin that is supposed to escort glucose molecules into the cells.
That’s why insulin resistance is the main factor in type 2 diabetes, and it all starts with poor diets and sedentary lifestyles. Of course, suppressed stress is another factor.
Type 2 diabetes is much more common than type 1 or insulin-dependent diabetes. It’s been on the rise largely due to the increased consumption of processed carbs and sugars in sodas, junk foods, and even high quality processed foods. They all contribute toward metabolic syndrome with obesity, high blood pressure, and hyperglycemia.
The point is that type 1 diabetes is not in the realm of dietary rescue by any known food substance. Its pancreatic malfunction needs an external supply of insulin to supply cells that are not insulin resistant, thus the term ‘insulin dependent’ applies to type 1 diabetes.
See:
Study: Insulin May Actually Accelerate Death in Type 2 Diabetes
Other studies referenced by researchers in this study mention success with VCO on rats whose diets were radically altered to create type 2 diabetes from metabolic syndrome, which the researchers concede. From the study text:
The importance of intestinal microbiome composition in the treatment of type 2 diabetes has been recently emphasized.
See:
Research Continues to Confirm Coconut Oil’s Healing Properties for Diabetes
This study was ostensibly concerned with the effect of coconut oil, a dietary solution that has proven itself for assisting with obesity and metabolic syndrome, a type 2 diabetes precursor.
Coconut oil does not seem to affect insulin levels directly if the type of diabetes induced by Alloxan resembles type 1 diabetes with suppressed pancreatic insulin production instead of a dietary/lifestyle-influenced metabolic syndrome that’s treatable by consuming virgin coconut oil and improving the overall diet.
If the pancreas beta cells are damaged or blocked, which Alloxan tends to do in order to simulate type 1 diabetes or insulin-dependent diabetes, then reversing insulin resistance or increasing insulin sensitivity would have little effect of lowering blood sugar, because not even enough insulin is being created to affect how sensitive to insulin those cells become.
Here’s one example of the type of study that used diet-induced metabolic syndrome rather than injected Alloxan to create diabetes symptoms. See:
Coconut Products Improve Signs of Diet-Induced Metabolic Syndrome in Rats
The effort to lower hyperglycemia resulting from cellular insulin resistance would come about by increasing cellular insulin sensitivity. This effort is enhanced with increased probiotic production, which was largely augmented with coconut oil consumption in this study and others.
See:




 The FDA has NOT Banned Trans Fats! Traditional Saturated Fats like Coconut Oil Continue to Shine for Alzheimer's Disease but are Condemned by U.S. Dietary Advice
The FDA has NOT Banned Trans Fats! Traditional Saturated Fats like Coconut Oil Continue to Shine for Alzheimer's Disease but are Condemned by U.S. Dietary Advice The Evidence of Coconut Oil's Superiority Over Drugs in Destroying Pathogens Continues to be Published in Peer-Reviewed Journals
The Evidence of Coconut Oil's Superiority Over Drugs in Destroying Pathogens Continues to be Published in Peer-Reviewed Journals Study: Virgin Coconut Oil Protects Neuronal Damage and Mortality after a Stroke Incidence
Study: Virgin Coconut Oil Protects Neuronal Damage and Mortality after a Stroke Incidence Another Phase 3 Trial Failure to Develop an Alzheimer's Drug Shows Why Virgin Coconut Oil is Needed to Prevent Dementia
Another Phase 3 Trial Failure to Develop an Alzheimer's Drug Shows Why Virgin Coconut Oil is Needed to Prevent Dementia FDA Food Police want to Dictate What Foods are "Healthy" in New Guidelines Criminalizing Traditional Fats Like Butter and Coconut Oil
FDA Food Police want to Dictate What Foods are "Healthy" in New Guidelines Criminalizing Traditional Fats Like Butter and Coconut Oil
Leave a Reply