
by Paul Fassa
Health Impact News
Headlines in the corporate-sponsored “mainstream” media recently warned the public about a new “mysterious infection” that is drug-resistant.
As a recent NY Times Health Section article reported, there is allegedly a hospital cover-up of an emerging candida fungus, Candida or C. auris.
It is the latest antimicrobial drug-resistant “super-bug” to emerge in hospitals and nursing homes. This time it’s not about bacteria, it’s a virulent form of Candida.
And while the corporate media, sponsored in a large degree by Big Pharma, will almost never report on natural solutions, there is hope for fighting fungal infections like Candida where drugs have failed.
One of the most beneficial natural products that fights and kills strains of Candida, according to peer-reviewed research over the past several years, is coconut oil.
A Major Factor That Has Contributed to Candida Overgrowth and C. Auris
It seems there are many who can carry this fungus on their skin without ill effects as long as it doesn’t get into the bloodstream.
Candida auris manages to develop and remain on any material. So an asymptomatic human carrier can bring this fungus into a hospital room where it can prey on the elderly and ill who have to stay for any length of time.
So far, this hospital-borne, antifungal drug-resistant C. auris is not threatening populations outside of hospitals and nursing homes where the more vulnerable elderly and sick live day to day.
Most of the Candida auris infections occurred in a few hospitals in England, Spain, parts of Asia, and now in the USA. But nearly half of the several hundred immunocompromised elderly and sick infected with C. auris have died. (Source)
The overuse of pharmaceutical antibiotics has led to a crisis of antibiotic, drug-resistant super-bugs. It’s known that a majority of pharma antibiotics are used on factory farm livestock as a pre-slaughter fattener and to protect them against the diseases from overcrowded, unnatural feeding conditions called CAFOs (concentrated animal feeding operations).
Enough antibiotics wind up in our food chain to create a tipping point for those who subsist on the Standard American Diet (SAD) which includes factory farm meat and dairy products retaining some levels of those antibiotics. Add this to overly-prescribed antibiotics.
What happens is pathogenic microbes mutate and develop resistance over time to those drugs. Perhaps it’s more a case of that antimicrobial drug no longer being able to identify its target.
Natural microbes can figure out how to avoid synthetic chemicals imposed on them. They have an ample supply of pharmaceutical antibiotic drugs to practice survival with. Apparently, pathogens haven’t grasped how to outsmart natural antimicrobial agents such as colloidal silver and coconut oil.
Perhaps even more importantly, those antibiotics harm and reduce the “good” bacteria in our microbiomes that serve and protect us. They wind up making us more vulnerable to infectious diseases or contribute toward auto-immune diseases, which are more on the rise than infectious diseases. (Source)
Most Candida overgrowth sufferers have had a history of antibiotic use. Candida yeast cells comprise a minority of our microbiome population. Normally, they’re kept in check by the majority of our beneficial bacteria.
But if antibiotics are used enough to significantly deplete the beneficial bacteria, those candida cells rapidly rise to overwhelm the microbiome balance and create a candida overgrowth.
Ironically, the overuse of antibiotics has also led to the rise of candida overgrowth known as Candida albicans, or yeast infections, and now this new antifungal-resistant Candida auris. See:
Pharmaceutical Antibiotic Drugs: Life Saver or Life Destroyer?
Antifungal drugs are not as commonly used for humans and animals as antibiotics. But two of the scientists interviewed in the NY Times article claim antifungal crop-spraying has been the major contributor toward creating this new antifungal drug resistance. (Source)
A 2013 study, Emergence of Azole-Resistant Aspergillus fumigatus Strains due to Agricultural Azole Use Creates an Increasing Threat to Human Health, carefully examined this situation. Azole-based fungicides are commonly used in agriculture.
Attempts at creating cocktails of existing antifungal drugs have proven to have little effect on Candida auris. Even if somewhat effective, antifungal drugs are packaged with some potentially nasty side effects.
What Coconut Oil Can Do for Candida Overgrowth
Coconut oil’s natural antifungal efficacy offers additional health benefits instead of adverse side effects. This is the prophylactic dynamic and part of the potential healing solution to this hyped-up candida danger.
Yet, there was no mention of this by the CDC or media regarding the sudden appearance of antifungal resistant Candida auris. Part of this is due to the official dogma of the cholesterol theory of heart disease, diabetes, and obesity over the past 50 plus years which has been proven false.
And coconut oil has been demonized as an unhealthy saturated fat.
But the saturated fat/cholesterol theory of heart disease, diabetes, and obesity is simply a false dogma based on faulty science, enforced by government and non-government agencies and bolstered by the processed low-fat food industry and promoted by mainstream media. There was a media exception. See:
Time Magazine: We Were Wrong About Saturated Fats
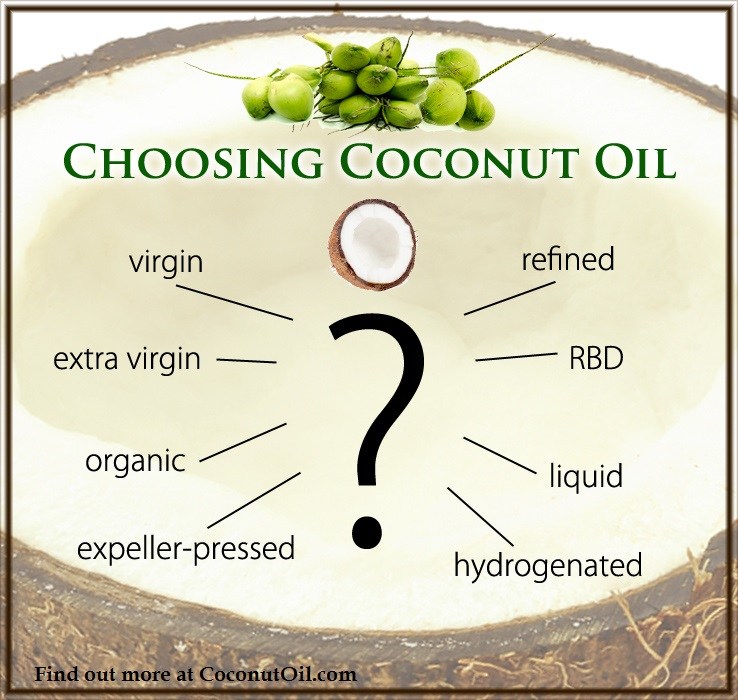
There have been many studies done on coconut oil and its beneficial fatty acids, mostly in other nations, that haven’t been given any mainstream media exposure in the U.S. The most potent beneficial fatty acids in coconut oil fighting candida overgrowth are:
- Caproic Acid
- Caprylic Acid
- Capric Acid
- Lauric Acid
A 2012 study in Japan, [Inhibition of Candida mycelia growth by a medium chain fatty acids, capric acid in vitro and its therapeutic efficacy in murine oral candidiasis], found all four fatty acids have pronounced antiseptic properties on candida fungi.
A Nigerian study in 2007, In vitro antimicrobial properties of coconut oil on Candida species in Ibadan, Nigeria, analyzed the antifungal properties of coconut oil compared to the pharmaceutical antifungal drug fluconazole, concluding:
Coconut oil should be used in the treatment of fungal infections in view of emerging drug-resistant Candida species. (Source)
Anecdotal successes with coconut oil have been reported at coconutoil.com. One person wrote:
It’s been 5 years that I have really been struggling with this (though the imbalance was established long before that). I read that taking …..Virgin Coconut Oil could help with a candida imbalance and it really has. (Source)
Another testified:
I’ve been battling a systemic candida yeast infection for over ten years. I have the mutated (fungal) stage and it’s the toughest thing I’ve ever had to deal with. … there are no phamaceuticals for it that are effective.
Candida yeast can overgrow in the gut under the right conditions until it mutates and becomes an invading pathogen, moves out of the gut and grows in mass in any part of the body.
When it affects a vital organ, then it can be deadly.
I’ve tried everything from conventional drugs to all the natural remedies … but have never experienced the “die-off effect,” or Herxheimer Reaction … symptoms generated by a detoxification process.
[This oil] is something I will not be without for the rest of my life. (Source)
More Studies on Coconut Oil for Fungal Yeast Infections
The efficacy of coconut oil for yeast infection suppression was tested at Tufts University in Massachusetts in 2015.
The study report advised looking more into coconut oil as a medical treatment for candida overgrowth issues to reduce writing prescriptions for antifungals.
Lead study author Kearney Gunsalus, PhD, explained:
The potential use of coconut oil in the short term to control the rate of fungal overgrowth should not be considered a prophylactic approach to preventing fungal infections.
We want to give clinicians a treatment option that might limit the need for antifungal drugs.
If we can use coconut oil as a safe, dietary alternative, we could decrease the amount of antifungal drugs used, reserving antifungal drugs for critical situations. (Source)
An earlier study examined caprylic acid, which is one of four fatty acids contained in coconut oil that are effective against candida overgrowth. It compared the results of caprylic acid with Diflucan, a pharmaceutical antifungal drug, concluding:
Caprylic acid is superior to & less expensive than Diflucan, [a pharmaceutical antifungal] & has potential application for anti-cancer, anti-aging, anti-Alzheimer’s disease, anti-Autism, anti-infection, & general circulatory improvement. (Source)
That’s quite a lot of medicinal power for only one of the four beneficial, easily-digested, medium chain fatty acids contained in coconut oil.
Dietary Assistance to Support Coconut Oil Efficacy
Many holistic doctors consider coconut oil as the “pesticide” part of a healing protocol involving a proper diet to support a gut microbiome population balance.
The dietary discipline usually involves greatly reducing sugar and refined carbohydrate intake and avoiding processed vegetable oils and margarine with trans-fatty acids and packaged foods with preservatives and MSG.
For most Candida sufferers, 3.5 tablespoons of virgin coconut oil daily may provide a sufficient pesticide for reducing candida growth to healthy gut microbiome parameters. But it should be supported by a proper diet. A ketogenic high fat low carb diet is an effective dietary solution.
At the very least, one should at least greatly minimize sugars and other simple or refined carbs that candida thrive on. Don’t fall for the artificial sweetener “solution” either. They are as bad or worse than sugars and high fructose corn syrup (HFCS).
Replace convenient processed foods with high quality, pure, whole foods, and don’t use microwave ovens for cooking or warming foods or liquids.
Add probiotic fermented foods to your daily food consumption to bolster the friendly benign bacteria’s population in your gut microbiome. It’s best to make your own milk or water kefir. You can order “starter grains” with instructions for making these kefirs online.
Prebiotic foods are what probiotic (friendly or good bacteria) thrive on. Surprisingly, starchy foods once cooked then cooled and consumed cold provide a prebiotic foundation to help support your probiotic bacteria.
Using only organic whole grains or potatoes is recommended by food and nutrition experts as the starchy foods to create this “resistant starch,” meaning it resists being broken down into glucose. Instead, it forms into a food source for probiotic bacteria. See:
Study: Candida Infections Can Be Controlled with Coconut Oil
Virgin Coconut Oil:
How it has changed people’s lives and how it can change yours!
Includes 85 recipes – Free shipping available!




 The FDA has NOT Banned Trans Fats! Traditional Saturated Fats like Coconut Oil Continue to Shine for Alzheimer's Disease but are Condemned by U.S. Dietary Advice
The FDA has NOT Banned Trans Fats! Traditional Saturated Fats like Coconut Oil Continue to Shine for Alzheimer's Disease but are Condemned by U.S. Dietary Advice The Evidence of Coconut Oil's Superiority Over Drugs in Destroying Pathogens Continues to be Published in Peer-Reviewed Journals
The Evidence of Coconut Oil's Superiority Over Drugs in Destroying Pathogens Continues to be Published in Peer-Reviewed Journals Study: Virgin Coconut Oil Protects Neuronal Damage and Mortality after a Stroke Incidence
Study: Virgin Coconut Oil Protects Neuronal Damage and Mortality after a Stroke Incidence Another Phase 3 Trial Failure to Develop an Alzheimer's Drug Shows Why Virgin Coconut Oil is Needed to Prevent Dementia
Another Phase 3 Trial Failure to Develop an Alzheimer's Drug Shows Why Virgin Coconut Oil is Needed to Prevent Dementia FDA Food Police want to Dictate What Foods are "Healthy" in New Guidelines Criminalizing Traditional Fats Like Butter and Coconut Oil
FDA Food Police want to Dictate What Foods are "Healthy" in New Guidelines Criminalizing Traditional Fats Like Butter and Coconut Oil
Leave a Reply