by Brian Shilhavy
Health Impact News
The US Government announced last year that they were doing away with the old food pyramid, and replacing it with a plate instead. One thing that has not changed, however, is the government’s low fat dietary advice, in spite of the abundance of research pointing in the other direction. Among the recommendations is to include “fat-free” or “low-fat” milk, for example. This is very dangerous advice, as the fat present in dairy is a necessary part of nutrition, especially for fat soluble vitamins such as Vitamin A and Vitamin D.
One of the criticisms still leveled against low-carb high-fat diets is that while studies exist showing their short-term benefits, there are no long-term studies. However, there are plenty of epidemiological studies of native populations consuming traditional foods showing the effectiveness of such dietary practices. The usual objection to such studies is that these “native” populations that consumed traditional diets prior to the introduction of processed foods led more active lifestyles which offset the harmful effects of eating too much fat. This is the most common objection I have received over the years when pointing out the abundance of positive studies on coconut oil in native cultures, for example. Such logic (or lack thereof) has always amazed me. Even if this theory was true, why not place the blame of modern disease on the sedentary lifestyle rather than traditional diets? If the two factors together (high-fat low-carb diets and sedentary lifestyles) cause disease, why blame the one that together with an active lifestyle apparently does not result in disease? The logic fails. Also, are we to assume that traditional cultures had no sedentary lazy people, or people of wealth that did not have to do manual labor? The logic fails again.
Interestingly, aside from the epidemiological studies on the long-term effects of a low-carb high-fat diet, I did find one study that has been around since 2004, and it is published right on the US Government National Institute of Health website. It is a study that was published in Experimental and Clinical Cardiology: Long-term effects of a ketogenic diet in obese patients. A lot of research has been published this year on just how therapeutic the extremely high-fat ketogenic diet is in fighting disease. So with all this research published, including this study on the government’s own website, showing the benefits of a high-fat diet, why does the government continue to promote the failed low-fat dietary advice? Here is the study:
| Exp Clin Cardiol. 2004 Fall; 9(3): 200–205. | PMCID: PMC2716748 |
Copyright © 2004, Pulsus Group Inc. All rights reserved
Clinical Cardiology
Long-term effects of a ketogenic diet in obese patients
Hussein M Dashti, MD PhD FICS FACS,1 Thazhumpal C Mathew, MSc PhD FRCPath,4 Talib Hussein, MB ChB,5 Sami K Asfar, MB ChB MD FRCSEd FACS,1 Abdulla Behbahani, MB ChB FRCS FACSI PhD FICS FACS,1 Mousa A Khoursheed, MB ChB FRCS FICS,1Hilal M Al-Sayer, MD PhD FICS FACS,1 Yousef Y Bo-Abbas, MD FRCPC,2 and Naji S Al-Zaid, BSc PhD3
1Departments of Surgery
2Medicine and
3Physiology, Faculty of Medicine, and
4Faculty of Allied Health Sciences, Kuwait University, Safat;
5Ministry of Health, Safat, Kuwait
Correspondence: Dr Naji Al-Zaid, Department of Physiology, Faculty of Medicine, PO Box 24923, 13110, Safat, Kuwait. Telephone 965-531-9593, fax 965-531-9597, e-mail alzaidnajeee@hotmail.com
Abstract
BACKGROUND:
Although various studies have examined the short-term effects of a ketogenic diet in reducing weight in obese patients, its long-term effects on various physical and biochemical parameters are not known.
OBJECTIVE:
To determine the effects of a 24-week ketogenic diet (consisting of 30 g carbohydrate, 1 g/kg body weight protein, 20% saturated fat, and 80% polyunsaturated and monounsaturated fat) in obese patients.
In the present study, 83 obese patients (39 men and 44 women) with a body mass index greater than 35 kg/m2, and high glucose and cholesterol levels were selected. The body weight, body mass index, total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, triglycerides, fasting blood sugar, urea and creatinine levels were determined before and after the administration of the ketogenic diet. Changes in these parameters were monitored after eight, 16 and 24 weeks of treatment.
RESULTS:
The weight and body mass index of the patients decreased significantly (P<0.0001). The level of total cholesterol decreased from week 1 to week 24. HDL cholesterol levels significantly increased, whereas LDL cholesterol levels significantly decreased after treatment. The level of triglycerides decreased significantly following 24 weeks of treatment. The level of blood glucose significantly decreased. The changes in the level of urea and creatinine were not statistically significant.
CONCLUSIONS:
The present study shows the beneficial effects of a long-term ketogenic diet. It significantly reduced the body weight and body mass index of the patients. Furthermore, it decreased the level of triglycerides, LDL cholesterol and blood glucose, and increased the level of HDL cholesterol. Administering a ketogenic diet for a relatively longer period of time did not produce any significant side effects in the patients. Therefore, the present study confirms that it is safe to use a ketogenic diet for a longer period of time than previously demonstrated.
Keywords: Diet, Ketosis, Obesity
Obesity has become a serious chronic disease in both developing and developed countries. Furthermore, it is associated with a variety of chronic diseases (1–4). It is estimated that in the United States alone approximately 300,000 people die each year from obesity-related diseases (5,6). Different methods for reducing weight using reduced calorie and fat intake combined with exercise have failed to show sustained long-term effects (7–9). Recent studies from various laboratories (10,11), including our own (12), have shown that a high fat diet rich in polyunsaturated fatty acids (ketogenic diet) is quite effective in reducing body weight and the risk factors for various chronic diseases. The ketogenic diet was originally introduced in 1920 (13). In this diet, the fat to carbohydrate ratio is 5:1. While there was a significant decrease in the weight of obese patients who were on a ketogenic diet (12), the reverse occurred when the diet changed to one high in carbohydrates (14).
It should be noted that the concept that fat can be eaten ad libitum and still induce weight loss in obese subjects is not a recent one (13–33). Ketosis occurs as a result of the change in the body’s fuel from carbohydrate to fat. Incomplete oxidation of fatty acids by the liver results in the accumulation of ketone bodies in the body. A ketogenic diet maintains the body in a state of ketosis, which is characterized by an elevation of D-b-hydroxybutyrate and acetoacetate.
Mild ketosis is a natural phenomenon that occurs in humans during fasting and lactation (19,20). Postexercise ketosis is a well-known phenomenon in mammals. Although most of the changes in the physiological parameters induced following exercise revert back to their normal values rapidly, the level of circulating ketone bodies increases for a few hours after muscular activity ceases (21). It has been found that in trained individuals, a low blood ketone level protects against the development of hypoglycemia during prolonged intermittent exercise (22). In addition, ketosis has a significant influence on suppressing hunger. Thus, a ketogenic diet is a good regulator of the body’s calorie intake and mimics the effect of starvation in the body.
It is generally believed that high fat diets may lead to the development of obesity and several other diseases such as coronary artery disease, diabetes and cancer. This view, however, is based on studies carried out in animals that were given a high fat diet rich in polyunsaturated fatty acids. In contrast, our laboratory has recently shown that a ketogenic diet modified the risk factors for heart disease in obese patients (12).
Although various short-term studies examining the effect of a ketogenic diet in reducing the weight of obese patients have been carried out (10), its long-term effects in obese subjects are not known (15). Therefore, the purpose of the present study was to investigate the long-term effects of a ketogenic diet on obesity and obesity-associated risk factors in a large population of obese patients.
PATIENTS AND METHODS
Patients and biochemical analysis
The prospective study was carried out at the Academic Department of Surgery, Consultation and Training Centre, Faculty of Medicine, Kuwait University (Jabriya, Kuwait) in 83 obese subjects (39 men and 44 women). The body mass index (BMI) of men and women was 35.9±1.2 kg/m2 and 39.4±1.0 kg/m2, respectively. The mean age was 42.6±1.7 years and 40.6±1.6 years for men and women, respectively. The mean age, initial height, weight and BMI for all patients are given in Table 1. Fasting blood tests were carried out for all of the subjects. Initially, all patients were subjected to liver and renal function tests, and glucose and lipid profiles, using fasting blood samples, and a complete blood count. Thereafter, fasting blood samples were tested for total cholesterol, high density lipoprotein (HDL) cholesterol, low density lipoprotein (LDL) cholesterol, triglycerides, blood sugar, urea and creatinine levels at the eighth, 16th and 24th week. In addition, weight and height measurements, and blood pressure were monitored at each visit.
|
|
TABLE 1
Patient data at baseline before treatment with the ketogenic diet
|
Protocol for ketogenic diet-induced body weight reduction
All 83 subjects received the ketogenic diet consisting of 20 g to 30 g of carbohydrate in the form of green vegetables and salad, and 80 g to 100 g of protein in the form of meat, fish, fowl, eggs, shellfish and cheese. Polyunsaturated and monounsaturated fats were also included in the diet. Twelve weeks later, an additional 20 g of carbohydrate were added to the meal of the patients to total 40 g to 50 g of carbohydrate. Micronutrients (vitamins and minerals) were given to each subject in the form of one capsule per day (Table 2).
|
|
TABLE 2
Composition of the capsule*
|
Statistical analysis
Statistical differences between body weight, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, level of fasting blood sugar, and urea and creatinine levels before and after the administration of the ketogenic diet were analyzed using a paired Student’s t test using the Stat-view version 4.02 (Abacus Concepts Inc, USA). Weight, BMI and all biochemical parameters are expressed as mean ± SEM.
RESULTS
The mean initial weight of the subjects was 101.03±2.33 kg. The weight decreased significantly during all stages of the treatment period. The body weights at the eighth, 16th and 24th week were 91.10±2.76 kg, 89.39±3.4 kg and 86.67±3.70 kg, respectively (Figure 1). Similar to the loss in body weight, a significant decrease was observed in the BMI of the patients following the administration of the ketogenic diet. The initial BMI, and the BMI after the eighth, 16th and 24th week were 37.77±0.79 kg/m2, 33.90±0.83 kg/m2, 33.24±1.00 kg/m2 and 32.06±1.13 kg/m2, respectively
(Figure 2).
|
|
Figure 1)
Reduction in body weight at eight, 16 and 24 weeks following the administration of the ketogenic diet in obese patients. The weights are expressed as mean ± SEM
|
|
|
Figure 2)
Decrease in body mass index at eight, 16 and 24 weeks during the administration of a ketogenic diet in obese patients. The values are expressed as mean ± SEM
|
The level of total cholesterol showed a significant decrease from week 1 to week 24 (Figure 3). The level of HDL cholesterol significantly increased (Figure 4), whereas LDL cholesterol levels significantly decreased with treatment (Figure 5). The level of triglycerides decreased significantly after 24 weeks of treatment. The initial level of triglycerides was 2.75±0.23 mmol/L, whereas at week 24, the level decreased to 1.09±0.08 mmol/L (Figure 6). The level of blood glucose significantly decreased at week 24. The initial blood glucose level and its level at the eighth, 16th and 24th week were 7.26±0.38 mmol/L, 5.86±0.27 mmol/L, 5.56±0.19 mmol/L and 5.62±0.18 mmol/L, respectively
(Figure 7). The changes in the levels of urea (Figure 8) and creatinine (Figure 9) were not statistically significant.
|
|
Figure 3) |
|
|
Figure 4)
Changes in the level of high density lipoprotein (HDL) cholesterol in obese patients during treatment with a ketogenic diet for a period of 24 weeks. Data are expressed as mean ± SEM
|
|
|
Figure 5)
Changes in the level of low density lipoprotein (LDL) cholesterol during treatment with a ketogenic diet in obese patients at eight, 16 and 24 weeks. The values are expressed as mean ± SEM
|
|
|
Figure 6)
Changes in the level of triglycerides in obese patients during treatment with a ketogenic diet over a period of 24 weeks. The values are expressed as mean ± SEM
|
|
|
Figure 7)
Decreased levels of blood glucose (expressed as mean ± SEM) in obese patients at eight, 16 and 24 weeks during the administration of a ketogenic diet
|
|
|
Figure
Changes in the level of urea in obese patients during a 24-week ketogenic diet. The level of urea is expressed as mean ± SEM
|
|
|
Figure 9)
Changes in the level of creatinine in obese patients during a 24-week ketogenic diet. Values are expressed as mean ± SEM
|
DISCUSSION
Until recently, ketosis was viewed with apprehension in the medical world; however, current advances in nutritional research have discounted this apprehension and increased public awareness about its favourable effects. In humans, ketone bodies are the only additional source of brain energy after glucose (23,24). Thus, the use of ketone bodies by the brain could be a significant evolutionary development that occurred in parallel with brain development in humans. Hepatic generation of ketone bodies during fasting is essential to provide an alternate fuel to glucose. This is necessary to spare the destruction of muscle from glucose synthesis.
A ketogenic diet is clinically and experimentally effective in antiepileptic and antiobesity treatments; however, the molecular mechanisms of its action remain to be elucidated. In some cases, a ketogenic diet is far better than modern anticonvulsants (25). Recently, it has been shown that a ketogenic diet is a safe potential alternative to other existing therapies for infantile spasms (27). It was further shown that a ketogenic diet could act as a mood stabilizer in bipolar illness (28). Beneficial changes in the brain energy profile have been observed in subjects who are on a ketogenic diet (28). This is a significant observation because cerebral hypometabolism is a characteristic feature of those who suffer from depression or mania (28). It has also been found that a ketogenic diet affects signal transduction in neurons by inducing changes in the basal status of protein phosphorylation (29). In another study (30), it was shown that a ketogenic diet induced gene expression in the brain. These studies provide evidence to explain the actions of a ketogenic diet in the brain.
One of the mechanisms of a ketogenic diet in epilepsy may be related to increased availability of beta-hydroxybutyrate, a ketone body readily transported through the blood-brain barrier. In support of this hypothesis, it was found that a ketogenic diet was the treatment of choice for glucose transporter protein syndrome and pyruvate dehydrogenase deficiency, which are both associated with cerebral energy failure and seizures (26).
One argument against the consumption of a high fat diet is that it causes obesity. The major concern in this regard is whether a high percentage of dietary fat promotes weight gain more than a low percentage of fat intake. Because fat has a higher caloric density than carbohydrate, it is thought that the consumption of a high fat diet will be accompanied by a higher energy intake (31). On the contrary, recent studies from our laboratory (12) and many other laboratories (24,32–34) have observed that a ketogenic diet can be used as a therapy for weight reduction in obese patients.
It has been found that a sugary diet is the root cause of various chronic diseases of the body. A recent study (35) showed that sugar can accelerate aging. Several recent studies (36,37) have pointed to the fact that a diet with a high glycemic load is independently associated with the development of cardiovascular diseases, type II diabetes and certain forms of cancer. Glycemic load refers to a diet of different foods that have a high glycemic index. Glycemic index is a measure of the elevation of glucose levels following the ingestion of a carbohydrate. The classification of a carbohydrate based on its glycemic index provided a better predictor of risk for coronary artery diseases than the traditional method of classification of carbohydrate into simple or complex forms (38). In other studies (38–46), it was shown that the risk of dietary glycemic load from refined carbohydrates was independent of other known risk factors for coronary diseases.
It is now evident that high carbohydrate diets increase fasting plasma triglyceride concentrations (47–51) and decrease HDL cholesterol concentrations (52–55). These changes are associated with enhanced atherogenesis (55). However, it has been shown that short-term ketogenic diets improve the lipid disorders that are characteristic of atherogenic dyslipidemia (56). It has also been found that sugary drinks decreased blood levels of vitamin E, thus reducing the amount of antioxidants in the body. It has been proven, beyond a doubt, that disrupting the oxidant-antioxidant status of the cell will lead to various diseases of the body (57).
The relation between a high fat diet and cancer is not conclusive. Recent epidemiological studies (17,58–60) could not explain a specific causal relationship between dietary fat and cancer. It has been found that altered energy metabolism and substrate requirements of tumour cells provide a target for selective antineoplastic therapy. The supply of substrates for tumour energy metabolism can be reduced by dietary manipulation (eg, ketogenic diet) or by pharmacological means at the cellular level (eg, inhibitors of glycolysis or oxidative phosphorylation). Both of these techniques are nontoxic methods for controlling tumour growth in vivo (61). Sugar consumption is positively associated with cancer in humans and test animals (58–61). This observation is quite logical because tumours are known to be enormous sugar absorbers. It has also been found that the risk of breast cancer decreases with increases in total fat intake (16). Further studies on the role of a ketogenic diet in antineoplastic therapy are in progress in our laboratory.
A link between low fat diets and osteoporosis has been suggested. Very low fat diets are considered to be low in calcium content. Women on low fat diets excrete most of the calcium they consume; therefore, they are more prone to osteoporosis. However, a high fat diet can rectify this situation (62).
In the present study, a control population on a low fat diet was not included due to the difficulties in recruiting subjects for a control group. However, several studies (63,64) with appropriate control groups that compared the effect of a low fat diet with a low carbohydrate ketogenic diet have recently been published. In this regard, these two recent studies are comparable with the present study. Brehm et al (23) showed that obese women on a low carbohydrate ketogenic diet lost 8.5 kg over six months compared with 4.2 kg lost by those in the low fat diet group (P<0.001). Twenty-two subjects from the low carbohydrate ketogenic diet and 20 subjects from the low fat diet completed the study, with both groups reducing their energy intake by approximately 450 kcal from the baseline level. In another study performed in 132 severely obese subjects for six months (24), there was greater weight loss in the low carbohydrate ketogenic diet group than in the low fat diet group (5.8 kg versus 1.9 kg, P=0.002). Both of these studies support the findings presented in the present paper.
CONCLUSIONS
The data presented in the present study showed that a ketogenic diet acted as a natural therapy for weight reduction in obese patients. This is a unique study monitoring the effect of a ketogenic diet for 24 weeks. There was a significant decrease in the level of triglycerides, total cholesterol, LDL cholesterol and glucose, and a significant increase in the level of HDL cholesterol in the patients. The side effects of drugs commonly used for the reduction of body weight in such patients were not observed in patients who were on the ketogenic diet. Therefore, these results indicate that the administration of a ketogenic diet for a relatively long period of time is safe. Further studies elucidating the molecular mechanisms of a ketogenic diet are in progress in our laboratory. These studies will open new avenues into the potential therapeutic uses of a ketogenic diet and ketone bodies.
REFERENCES
Articles from Experimental & Clinical Cardiology are provided here courtesy of
Pulsus Group
Article Source: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2716748/
Virgin Coconut Oil:
How it has changed people’s lives and how it can change yours!
Includes 85 recipes – Free shipping available!













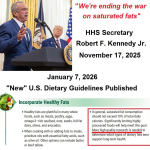 HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines
HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines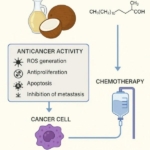 Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer
Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits
Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives
How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth
New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth