
by Dr. Mercola
One in four Americans aged 45 and older take statin drugs to lower cholesterol and supposedly “prevent heart disease.”
That amounts to 32 million Americans or, as Peter Wehrwein pointed out in the Harvard Health Letter, the equivalent of the entire populations of Florida and Illinois combined.i
If you’re one of these millions, or if you’re considering starting a statin prescription anytime soon, you should know that there are serious risks involved with taking these drugs, a fact that even the U.S. Food and Drug Administration (FDA) is now acknowledging.
Evidence includes diaries, court records, medical books and literature, in which these two sleep cycles are referred to in such a way as to make it clear that it was common knowledge at the time.
FDA Adds New Warning Labels to Statin Drugs
Following an internal meeting between the FDA’s Office of Surveillance and Epidemiology and Office of New Drugs, the Agency announced it would be requiring additional warning labels for statin drugs. Among them are warnings that statins may increase the risk of:
- Liver damage
- Memory loss and confusion
- Type 2 diabetes
- Muscle weakness (for certain statins)
According to Dr. Amy Egan, the FDA’s deputy director of safety in the division of metabolism drug products, the new warnings, particularly the one for memory loss, came as the result of anecdotal reports compiled over the past year. In short, with well over 30 million Americans now taking statin drugs, we’re witnessing a massive ongoing ‘live’ experiment, and many are putting their health on the line for drugs that offer little in the way of heart protection. In fact, they may actually make your heart health worse.
Where’s the Warning for CoQ10 Depletion?
Though the FDA has added new warnings to statin labels, they are continuing to sing their praises and still made sure to tell ABC News “We still think the benefits of the drug outweigh the risks.” These warnings are long overdue, as the drugs are being prescribed to tens of millions of Americans who do not need them, and who are being kept largely in the dark about their potential risks. But they do not go far enough to adequately protect the public.
Ironically, while reducing your risk of cardiovascular events and heart disease is the primary motivation for prescribing statins, these drugs can actually increase your risk of heart disease because they deplete your body of Coenzyme Q10 (CoQ10), which can lead to heart failure. Statins lower your CoQ10 levels by blocking the pathway involved in cholesterol production — the same pathway by which Q10 is produced. Statins also reduce the blood cholesterol that transports CoQ10 and other fat-soluble antioxidants.
The loss of CoQ10 leads to loss of cell energy and increased free radicals which, in turn, can further damage your mitochondrial DNA, effectively setting into motion a health-destroying circle of increasing free radicals and mitochondrial damage.
There are no official warnings in the United States regarding CoQ10 depletion from taking statin drugs, and many physicians fail to inform you about this problem as well. Labeling in Canada, however, clearly warns of CoQ10 depletion and even notes that this nutrient deficiency “could lead to impaired cardiac function in patients with borderline congestive heart failure.”
As your body gets more and more depleted of CoQ10, you may suffer from fatigue, muscle weakness and soreness, and eventually heart failure, so it is imperative if you take statin drugs that you take CoQ10 or, if you are over the age of 40, or subject to excessive oxidative stress, the reduced version called ubiquinol. A simple warning as such could save countless numbers of people from this potentially deadly risk … but the FDA has stayed mum.
FDA Removes One Important Safety Warning
Due to statins’ potential to increase liver enzymes and cause liver damage, patients must be monitored for normal liver function. At least, that’s what the label used to say. Now the FDA has removed this long-standing warning and ruled that patients taking statins no longer need routine monitoring of liver enzymes, but instead can have liver enzymes tested before starting the drugs, and then only as clinically needed. It’s unclear what prompted the FDA to remove the warning, but many physicians have told the press they plan to continue monitoring their patients’ liver enzymes anyway.
ABC News reported:
“I disagree with the notion that you can stop checking for liver function test abnormalities,” said Dr. Andrew Carroll, a physician at the Renaissance Medical Group in Phoenix. Carroll said he saw high liver enzymes in about 5 percent of the patients to whom he prescribed statins, prompting him to recommend they stop taking the medication.”
It makes no sense that the FDA would remove this cautionary warning, as statins are linked to severe liver injury. Of all the adverse drug reactions (ADRs) suspected to be due to statins received by the Swedish Adverse Drug Reactions Advisory Committee from 1988-2010, the most common was drug-induced liver injury.ii Such cases accounted for 57 percent of all the statin-related ADRs and included potentially severe, and in some cases deadly, consequences, including:
- Deaths from acute liver failure
- Liver transplantation
- Jaundice
The link to liver damage was quite strong, and in several cases after patients recovered from the initial liver damage and then started taking statins again, a similar pattern of liver injury occurred. If someone you love is currently taking a statin, please do alert them to this potential danger, as it can occur quickly. Most patients experienced liver injury just three to four months after the start of therapy.
Further, in 2010 data from more than 2 million 30- to 84-year-old statin users from England and Wales identified increased risks of moderate or serious liver dysfunction as well, among other serious effects, including acute kidney failure, moderate or serious myopathy (muscle disease), and cataract.iii
How Big of a Risk are Statins for Memory Problems and Diabetes?
Statins appear to provoke serious risks of chronic disease, including diabetes, through a few different mechanisms. One primary mechanism is by increasing your insulin levels, which can be extremely harmful to your health. Chronically elevated insulin levels cause inflammation in your body, which is the hallmark of most chronic disease. In fact, elevated insulin levels lead to heart disease, which, ironically, is the primary reason for taking a statin drug in the first place!
It can also promote belly fat, high blood pressure, heart attacks, chronic fatigue, thyroid disruption, and diseases like Parkinson’s, Alzheimer’s, and cancer.
Statins also increase your diabetes risk by raising your blood sugar. When you eat a meal that contains starches and sugar, some of the excess sugar goes to your liver, which then stores it away as cholesterol and triglycerides. Statins work by preventing your liver from making cholesterol. As a result, your liver returns the sugar to your bloodstream, which raises your blood sugar levels.
These drugs also rob your body of certain valuable nutrients, which can also impact your blood sugar levels. Two nutrients in particular, vitamin D and CoQ10, are both needed to maintain ideal blood glucose levels.
A recent meta-analysis confirmed that statin drugs are indeed associated with increased risk of developing diabetes.
The researchers evaluated five different clinical trials that together examined more than 32,000 people. They found that the higher the dosage of statin drugs being taken, the greater the diabetes risk. The “number needed to harm” for intensive-dose statin therapy was 498 for new-onset diabetes — that’s the number of people who need to take the drug in order for one person to develop diabetes. In other words, one out of every 498 people who are on a high-dose statin regimen will develop diabetes. If you factor in all 32 million people taking statins, that’s over 64,000 cases of diabetes!
Are Hundreds of Side Effects Being Ignored?
The FDA’s new warning labels may open some people’s eyes to a couple of new statin risks … but what about all the rest of them? Consumer health groups like Natural Society have pointed out that hundreds of adverse health effects have been linked to the drugs, and patients are largely kept in the dark about these risks. As noted in a Natural Society press release:iv
“Fundamentally, the research indicates that statin drugs damage the muscles and nerves in the body. There are well over 100 studies demonstrating the myotoxic, or muscle-harming effects of these drugs, and over 80 demonstrating the nerve-damaging effects. Since the heart is such a vital muscle innervated by a complex network of nerves, many healthcare providers now seriously question whether the unintended, unwanted side effects of statins are worse than the purported “cardiovascular” benefits they provide. Therefore, these peer reviewed research studies may also explain why rates of heart failure may be increasing in the general population who are given these drugs.
While the discovery that statin drugs, instead of preventing heart disease likely contributes to it, might be surprising, it should not distract from the more disturbing discovery that they contribute to over 300 disease and/or adverse health effects.”
That’s right — statin drugs have been directly linked to over 300 side effects, which include:
| Cognitive loss | Neuropathy | Anemia |
| Acidosis | Frequent fevers | Cataracts |
| Sexual dysfunction | An increase in cancer risk | Pancreatic dysfunction |
| Immune system suppression | Muscle problems, polyneuropathy (nerve damage in the hands and feet), and rhabdomyolysis, a serious degenerative muscle tissue condition | Hepatic dysfunction. (Due to the potential increase in liver enzymes, patients must be monitored for normal liver function) |
For more information about cholesterol, and why conventional advice to reduce your cholesterol to ridiculously low levels is foolhardy, please listen to this interview with Dr. Stephanie Seneff.



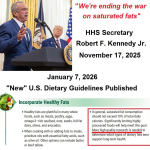 HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines
HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines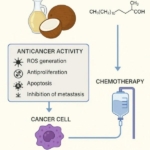 Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer
Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits
Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives
How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth
New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth