By Dr. Mercola
About one in three Americans now has diabetes or pre-diabetes. That’s nearly 80 million people, the majority of whom suffer from type 2 diabetes – a preventable and, often, reversible condition.
The problem is that many Americans are unaware that the foods they’re eating could be setting them up for a dietary disaster, and this isn’t their fault. Public health guidelines condemn healthy fats from foods like butter and full-fat dairy and recommend whole grains and cereals – the opposite of what a person with diabetes, or any person really, needs to stay healthy.
For the last 50 years, Americans have been told to eat a high complex carbohydrate, low saturated fat diet. Even diabetics have been told to eat 50 to 60 percent of their daily calories in the form of processed carbs!
Research, including a new study involving dolphins, again suggests that this movement away from traditional full-fat foods is contributing to the rising rates of diabetes and metabolic syndrome across the globe.
Dolphin Study Suggests Saturated Fats Are Beneficial for Diabetes
Researchers from the National Marine Mammal Foundation (NMMF) discovered that dolphins are able to switch in and out of a diabetes-like state, as well as develop metabolic syndrome, a cluster of symptoms that is often indicative of pre-diabetes in humans (and a sign that full-blown diabetes, and other conditions like heart disease, may not be far off).
To determine what might be driving metabolic syndrome in the dolphins, the researchers looked into their diet, which is primarily fish.1 It turned out that the saturated fat heptadecanoic acid was most beneficial for metabolism, and dolphins with the highest levels in their blood had lower insulin and triglyceride levels.2
Several dolphins with low heptadecanoic acid levels were then fed fish high in the saturated fat. Within six months, their markers of metabolic syndrome, including elevated insulin, glucose, and triglycerides, were normal.
Also striking, elevated levels of ferritin (iron), which is a precursor to metabolic syndrome, were also lowered within three weeks of the high saturated fat diet. The fish in the study with the highest level of heptadecanoic acid (also known as margaric acid or C17:0) was mullet – but it’s also found in whole fat dairy products, including whole milk, whole milk yogurt, and butter (non-fat dairy products had no detectable amounts of heptadecanoic acid).
Study author Dr. Stephanie Venn-Watson, director of NMMF’s Translational Medicine and Research Program, told Science Daily:3
“We hypothesize that widespread movement away from whole fat dairy products in human populations may have created unanticipated heptadecanoic acid deficiencies… and, in turn, this dietary deficiency may be playing a role in the global diabetes pandemic.”
Butter May Reduce Your Diabetes Risk
While many people with diabetes think they’re following sound nutritional advice by shunning butter in favor of whole grain, the opposite is actually true. Butter need not be shunned and, in fact, is a beneficial source of healthy saturated fats, especially when it’s raw, organic, and grass-fed.
In the dolphin study, butter was found to be particularly high in the beneficial heptadecanoic acid, so perhaps it’s not surprising that past research has also linked it to a lower diabetes risk.
The study included nearly 27,000 people between the ages of 45 to 74 who were followed for 14 years. Those who ate eight portions of full-fat dairy products a day cut their risk of diabetes by nearly 25 percent compared to those who ate fewer portions.4 According to lead author Dr. Ulrika Ericson of the Lund University Diabetes Center in Malmö, Sweden:5
“Our observations may contribute to clarifying previous findings regarding dietary fats and their food sources in relation to type 2 diabetes. The decreased risk at high intakes of high-fat dairy products, but not of low-fat dairy products, indicate that dairy fat, at least partly, explains observed protective associations between dairy intake and type 2 diabetes…”
In 2010, a study published in the Annals of Internal Medicine proposed that it’s the palmitoleic acid, which occurs naturally in full-fat dairy products, that protects against insulin resistance and diabetes.
People who consumed full-fat dairy had higher levels of trans-palmitoleate in their blood, and this translated to a two-thirds lower risk of developing type 2 diabetes compared to people with lower levels.6
Replacing Saturated Fats with Carbs Leads to Diabetes and Other Chronic Diseases
The American Heart Association began encouraging Americans to limit dietary fat, particularly animal fats, in order to reduce their risk of heart disease as far back as 1961.
Yet research has been pouring in refuting the saturated fat/heart disease link while linking processed carbs to higher rates of disease. As of 2015, the current dietary recommendations from the US Department of Agriculture (USDA) still make no distinction between healthy saturated fats and decidedly unhealthy synthetic trans fats in your diet.
Every five years, the US Departments of Agriculture (USDA) and Health and Human Services (HHS) convene a 15-member panel to update the nation’s dietary guidelines.
The Dietary Guidelines Advisory Committee (DGAC) scientific report is an important part of this process, and this year’s report finally acknowledged “Dietary advice should put the emphasis on optimizing types of dietary fat and not reducing total fat.”7 As noted by Forbes:8
“[T]he recommendation to have no more than 35 percent of your calories coming from fats is over. ‘Placing limits on total fat intake has no basis in science and leads to all sorts of wrong industry and consumer decisions,’ said Dariush Mozaffarian, one of the authors of the new [JAMA] paper. 9
Modern evidence clearly shows that eating more foods rich in healthful fats like nuts, vegetable oils, and fish have protective effects, particularly for cardiovascular disease.
Other fat-rich foods, like whole milk and cheese, appear pretty neutral; while many low-fat foods, like low-fat deli meats, fat-free salad dressing, and baked potato chips, are no better and often even worse than full-fat alternatives. It’s the food that matters, not its fat content.”
Evidence of this was highlighted in an editorial in the journal Open Heart.10 In it, research scientist and doctor of pharmacy James J. DiNicolantonio reviews the cardiometabolic consequences of replacing saturated fats with carbohydrates, which includes the following:
- Shift to overall atherogenic lipid profile (lower HDL, increased triglycerides, and increased ApoB/ApoA-1 ratio)
- Increased risk of coronary heart disease, cardiovascular events, and death from heart disease and increased overall mortality (all causes)
- Increased thrombogenic markers
- Increased oxidized LDL
- Increased inflammation
- Reduced HDL
- Impaired glucose tolerance, higher body fat, weight gain, obesity, and diabetes
- Increased small, high-density LDL particles
- Increased risk for cancer
Why Too Many Carbs Trigger Type 2 Diabetes…
The underlying problem in type 2 diabetes is improper insulin and leptin signaling. In type 2 diabetes, your pancreas is still producing some insulin — in fact, usually too much insulin is being produced on a chronic basis — but your pancreas is unable to recognize the insulin and use it properly.
This is an advanced stage of insulin resistance, which is typically caused by a diet that is too high in sugars and sugar-forming foods such as grains. Type 2 diabetes also involves malfunction of leptin signaling, which is caused by chronically elevated insulin and leptin levels — again due to a diet that is too high in sugar.
It’s important to understand what really happens when you simply add insulin without addressing the underlying insulin/leptin resistance. When your blood sugar becomes elevated, insulin is released to direct the extra energy (sugar) into storage. A small amount is stored as a starch called glycogen, but the majority is stored as fat.
Insulin’s primary role is not to lower your blood sugar, but rather to store this extra energy as fat for future needs when food may not be available. The fact that insulin lowers your blood sugar is merely a “side effect” of this energy storage process. So taking more insulin just makes you fatter!
Saturated Fat Health Benefits
The latest science suggests healthy fats (saturated and unsaturated fats from whole food, animal, and plant sources) should comprise anywhere from 50 to 85 percent of your overall energy intake. Saturated fats provide a number of important health benefits, including the following:
- Providing building blocks for cell membranes, hormones, and hormone-like substances
- Mineral absorption, such as calcium
- Carriers for important fat-soluble vitamins A, D, E, and K
- Conversion of carotene into vitamin A
- Helping to lower cholesterol levels (palmitic and stearic acids)
- Acts as antiviral agent (caprylic acid)
- Optimal fuel for your brain
- Provides satiety
- Modulates genetic regulation and helps prevent cancer (butyric acid)
Further, it’s becoming increasingly clear that the same pathological process that leads to insulin resistance and type 2 diabetes may also hold true for your brain. As you over-indulge on sugar and grains, your brain becomes overwhelmed by the consistently high levels of glucose and insulin that blunts its insulin signaling, leading to impairments in your thinking and memory abilities, eventually causing permanent brain damage.
Alzheimer’s disease has even been dubbed “type 3 diabetes.” Here again, saturated fats play a role, as they are crucial for healthy brain function. This mistaken fat phobia has undoubtedly played a significant role in the dramatic rise in dementia and other neurological disorders along with type 2 diabetes, because your brain cannot function properly without fats. In fact, most people benefit from up to 50 to 85 percent of their daily calories in the form of fats for optimal health while they are seeking to resolve their insulin resistance.
A Tried-and-True Plan to Reverse Type 2 Diabetes: All the Healthy Fats You Want
Type 2 diabetes represents the vast majority of all diabetics, and contrary to conventional medical and media teaching, it’s nearly 100 percent curable through lifestyle changes alone. The following nutrition and lifestyle modifications should be the foundation of your diabetes prevention and treatment plan. Also, make sure to monitor your FASTING insulin level. This is every bit as important as monitoring your fasting blood sugar. You’ll want your fasting insulin level to be between 2 and 4.
The higher your level, the greater your insulin resistance and the more aggressive you need to be in your treatment plan, especially when it comes to altering your diet. As you’ll see, a focus on reducing sugars and grains and increasing healthy fats is center to this plan.
Swap out processed foods, all forms of sugar — particularly fructose — as well as all grains, for whole, fresh food. A primary reason for the failure of conventional diabetes treatment over the last 50 years has to do with seriously flawed dietary recommendations. Fructose, grains, and other sugar-forming starchy carbohydrates are largely responsible for your body’s adverse insulin reactions, and all sugars and grains — even “healthy” grains such as whole, organic ones — need to be drastically reduced.
If you’re insulin/leptin resistant, have diabetes, high blood pressure, heart disease, or are overweight, you’d be wise to limit your total fructose intake to 15 grams per day until your insulin/leptin resistance has resolved. This includes about 80 percent of Americans. For all others, I recommend limiting your daily fructose consumption to 25 grams or less, to maintain optimal health. The easiest way to accomplish this is by swapping processed foods for whole, ideally organic foods. This means cooking from scratch with fresh ingredients.
Processed foods are the main source of all the primary culprits, including high fructose corn syrup and other sugars, processed grains, trans fats, artificial sweeteners, and other synthetic additives that may aggravate metabolic dysfunction. Besides fructose, trans fat (NOT saturated fat) increases your risk for diabetes by interfering with your insulin receptors. Healthy saturated fats do not do this. Since you’re cutting out a lot of energy (carbs) from your diet when you reduce sugars and grains, you need to replace them with something. The ideal replacement is a combination of:
Low-to-moderate amount of high-quality protein. Substantial amounts of protein can be found in meat, fish, eggs, dairy products, legumes, and nuts. When selecting animal-based protein, be sure to opt for organically raised, grass-fed or pastured meats, eggs, and dairy, to avoid potential health complications caused by genetically engineered animal feed and pesticides. Most Americans eat far too much protein, so be mindful of the amount. I believe it is the rare person who really needs more than one-half gram of protein per pound of lean body mass.
Those that are aggressively exercising or competing and pregnant women should have about 25 percent more, but most people rarely need more than 40 to 70 grams of protein a day. To determine your lean body mass, find out your percent body fat, and subtract from 100. This means that if you have 20 percent body fat, you have 80 percent lean body mass. Just multiply that by your current weight to get your lean body mass in pounds or kilos. The chart below shows some common foods and their protein content:
- Red meat, pork, poultry, and seafood average 6 to 9 grams of protein per ounce. An ideal amount for most people would be a 3-ounce serving of meat or seafood (not 9 or 12-ounce steaks!), which will provide about 18 to 27 grams of protein
- Eggs contain about 6 to 8 grams of protein per egg. So an omelet made from two eggs would give you about 12 to 16 grams of protein. If you add cheese, you need to calculate that protein in as well (check the label of your cheese)
- Seeds and nuts contain on average 4 to 8 grams of protein per quarter cup
- Cooked beans average about 7 to 8 grams per half cup
- Cooked grains average 5 to 7 grams per cup
- Most vegetables contain about 1 to 2 grams of protein per ounce
As much high-quality healthy fat as you want (saturated and monounsaturated). For optimal health, most people need upwards of 50 to 85 percent of their daily calories in the form of healthy fats. Good sources include coconut and coconut oil, avocados, butter, nuts, and animal fats. (Remember, fat is high in calories while being small in terms of volume. So when you look at your plate, the largest portion would be vegetables.)
As many non-starchy vegetables as you want
Exercise regularly and intensely. Studies have shown that exercise, even without weight loss, increases insulin sensitivity.11High-intensity interval training (HIIT), which is a central component of my Peak Fitness program, has been shown to improve insulin sensitivity by as much as 24 percent in just four weeks.
Improve your omega-3 to omega-6 ratio. Today’s Western diet has far too many processed and damaged omega-6 fats, and is far too little omega-3 fats. The main sources of omega-6 fats are corn, soy, canola, safflower, peanut, and sunflower oil (the first two of which are typically genetically engineered as well, which further complicates matters). The optimal ratio of omega-6 to omega-3 is 1:1. However, our ratio has deteriorated to between 20:1 and 50:1 in favor of omega-6. This lopsided ratio has seriously adverse health consequences.
To remedy this, reduce your consumption of vegetable oils (this means not cooking with them and avoiding processed foods), and increase your intake of animal-based omega-3, such as krill oil. Vegetable-based omega-3 is also found in flaxseed oil and walnut oil, and it’s good to include these in your diet as well. Just know they cannot take the place of animal-based omega-3s.
Maintain optimal vitamin D levels year-round. Evidence strongly supports the notion that vitamin D is highly beneficial for diabetes. The ideal way to optimize your vitamin D level is by getting regular sun exposure or by using a high-quality tanning bed. As a last resort, consider oral supplementation with regular vitamin D monitoring to confirm that you are taking enough vitamin D to get your blood levels into the therapeutic range of 50 to 70 ng/ml. Also please note that if you take supplemental vitamin D, you create an increased demand for vitamin K2.
Get adequate high-quality sleep every night. Insufficient sleep appears to raise stress and blood sugar, encouraging insulin and leptin resistance, and weight gain. In one 10-year long study of 70,000 diabetes-free women, researchers found that women who slept less than five hours or more than nine hours each night were 34 percent more likely to develop diabetes symptoms than women who slept seven to eight hours each night.12 If you are having problems with your sleep, try the suggestions in my article “33 Secrets to a Good Night’s Sleep.”
Maintain a healthy body weight. If you incorporate the diet and lifestyle changes suggested above you will greatly improve your insulin and leptin sensitivity, and a healthy body weight will follow in time. Determining your ideal body weight depends on a variety of factors, including frame size, age, general activity level, and genetics. As a general guideline, you might find a hip-to-waist size index chart helpful. This is far better than BMI for evaluating whether or not you may have a weight problem, as BMI fails to factor in both how muscular you are, and your intra-abdominal fat mass (the dangerous visceral fat that accumulates around your inner organs), which is a potent indicator of leptin sensitivity and associated health problems.
Incorporate intermittent fasting. If you have carefully followed the diet and exercise guidelines and still aren’t making sufficient progress with your weight or overall health, I strongly recommend incorporating intermittent fasting. This effectively mimics the eating habits of our ancestors, who did not have access to grocery stores or food around the clock. They would cycle through periods of feast and famine, and modern research shows this cycling produces a number of biochemical benefits, including improved insulin/leptin sensitivity, lowered triglycerides and other biomarkers for health, and weight loss.
Intermittent fasting is by far the most effective way I know of to shed unwanted fat and eliminate your sugar cravings. Keep up your intermittent fasting schedule until your insulin/leptin resistance improves (or your weight, blood pressure, cholesterol ratios, or diabetes normalizes). After that, you only need to do it “as needed” to maintain your healthy state.
Optimize your gut health. Your gut is a living ecosystem, full of both good bacteria and bad. Multiple studies have shown that obese people have different intestinal bacteria than lean people. The more good bacteria you have, the stronger your immune system will be and the better your body will function overall. Fortunately, optimizing your gut flora is relatively easy. You can reseed your body with beneficial bacteria by regularly eating fermented foods (like natto, raw organic cheese, miso, and cultured vegetables).
Read the full article here.
Sources and References:
- 1 PLOS One July 22, 2015
- 2 3 Science Daily July 22, 2015
- 4 5 Telegraph September 16, 2014
- 6 Annals of Internal Medicine 2010 Dec 21;153(12):790-9
- 7 JAMA June 2015;313(24):2421-2422, The 2015 US Dietary Guidelines
- 8 Forbes June 24, 2015
- 9 JAMA June 2015;313(24):2421-2422, The 2015 US Dietary Guidelines
- 10 Open Heart March 5, 2014
- 11 Diabetologia. 2014 May;57(5):927-34
- 12 Greenmedinfo.com June 28, 2014



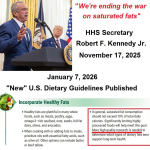 HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines
HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines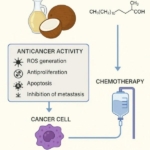 Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer
Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits
Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives
How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth
New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth
Leave a Reply