Health Impact News Editor Comments:
Recent advice proposed by the British NICE – the National Institute for Health and Care Excellence – is advocating that 15 million more people in the UK, most with no history of heart disease, should be taking cholesterol-lowering statin drugs.
Unintentionally, this move may have done more to educate people on the dangers of statin drugs than anything previously published in the alternative media, which has been warning people against the dangers of statin drugs for many years now. Popular doctors in the UK who go against the mainstream medical system in the UK have found willing publishers in the mainstream media in recent days, to publish the other side of the “statin wonder drug” hype that now wants to put almost 25% of the UK population on medications with known and published side effects and little to no benefits.
Suddenly, statin drug whistle blowers in the U.K., such as Dr. Malcolm Kendrick, are getting op-ed pieces in mainstream media. Dr. Kendrick had an article published in the Guardian yesterday: Statins aren’t a wonder drug – The claims made for statins are overblown. They are not a cure for most of the major diseases afflicting western civilisation.
Even mainstream medical doctors are starting to speak out, such as Dr. Kailash Chand, deputy chairman of the British Medical Association. He recently spoke out against the NICE proposal, stating that he also had suffered “awful” muscle pains while taking statins, and that plans to prescribe them to millions more adults will “only benefit drug companies”. (See: Deputy Chairman of British Medical Association Condemns Statins).
Add to this chorus of voices now vascular surgeon Dr Haroun Gajraj, who wrote an op-ed piece in theTelegraph yesterday. The British population is certainly getting an education on the other side of the story regarding statin drugs, but don’t expect to read about this in the pro-Pharma U.S. mainstream media.
Why I’ve ditched statins for good
by Dr Haroun Gajraj
The Telegraph
Excerpts:
When I had a routine health check-up eight years ago, my cholesterol was so high that the laboratory thought there had been a mistake. I had 9.3 millimoles of cholesterol in every litre of blood — almost twice the recommended maximum.
It was quite a shock. The GP instantly prescribed statins, the cholesterol-lowering drugs that are supposed to prevent heart disease and strokes. For eight years, I faithfully popped my 20mg atorvastatin pills, without side effects. Then, one day last May, I stopped. It wasn’t a snap decision; after looking more closely at the research, I’d concluded that statins were not going to save me from a heart attack and that my cholesterol levels were all but irrelevant.
When I informed my GP of my decision three months later, I wasn’t entirely honest. Rather than say I was skeptical about the drugs, I told my doctor I’d quit the statins because they were causing pain in my arm.
The GP simply suggested I try another brand of statin. The sooner the better, he said, given that I’d already been off my prescription for three months. “Hang on,” I said. “Could you give me a blood test first?” When the results came back, he was amazed that my total blood cholesterol was lower than when I’d been on statins. After three months without the pills, it was 5.4mmol/l (5.4 millimoles per litre of blood) compared with 5.7 mmol/l a year earlier.
The only major changes I’d made to my lifestyle since coming off statins were eliminating sugar (including alcohol and starchy foods such as bread) and eating more animal fat. Many experts now believe that sugar is emerging as a true villain in the heart-disease story; while after decades of demonisation, saturated fat has been acquitted of causing heart disease by a recent “meta” analysis of 70 studies by Cambridge University.
Typically, I was eating red meat three or four times a week and enjoying butter, full-fat milk and plenty of eggs. You would have thought that after three months on a diet so high in saturated fat, my cholesterol would have shot back up to pre-statin levels — but no, it came down and has stayed down seven months on. Not only that, but my levels of LDL (so-called bad cholesterol) were also lower than when I’d been on statins, and my ratio of HDL (so-called good cholesterol) to LDL was under four for the first time, an excellent sign, according to medical wisdom.
Continue Reading the Story Here.




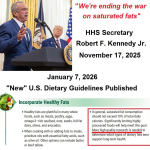 HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines
HHS Secretary Kennedy Breaks His Promise: "War on Saturated Fat" Kept in Tact with New U.S. Dietary Guidelines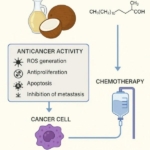 Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer
Research Continues to Show Virgin Coconut Oil's Effectiveness in Treating Cancer Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits
Coconut Oil Continues to Benefit Alzheimer's Patients over Drugs as Studies Continue for Neurological Benefits How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives
How the Simple High-Fat Low-Carb Ketogenic Diet Continues to Change People's Lives New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth
New Studies Continue to Show that Coconut Oil is the Best Oil for Treating Skin Conditions and Maintaining Healthy Skin and Teeth