By Dr. Mercola
Back in 2011, I published a series of interviews with Dr. Stephanie Seneff, a senior MIT research scientist who, more recently, rocked the world with her discovery of glyphosate’s mechanism of harm.
Three years ago, however, she was one of the first to point out the links between cholesterol and vitamin D, presenting a hypothesis that made me even more convinced that raising your vitamin D levels through sun exposure may be far more critical than previously thought.
Now, research published in the journal Menopause appears to offer support for Dr. Seneff’s theories on the cholesterol-vitamin D link. But first, a quick review of cholesterol, and why your body actually needs it.
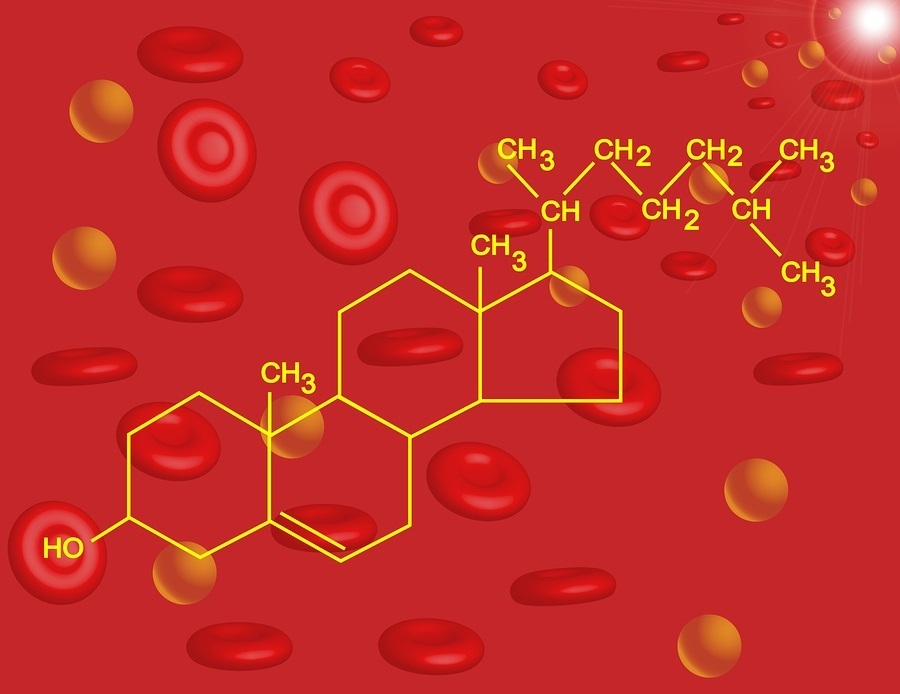
What Is Cholesterol, and Why Do You Need It?
That’s right, you do need cholesterol. This soft, waxy substance is found not only in your bloodstream but also in every cell in your body, where it helps to produce cell membranes, hormones, vitamin D, and bile acids that help you digest fat.
Cholesterol also helps in the formation of your memories and is vital for neurological function. Your liver makes about three-quarters or more of your body’s cholesterol, and according to conventional medicine, there are two types:
- High-density lipoprotein or HDL: This is the “good” cholesterol that helps keep cholesterol away from your arteries and remove any excess from arterial plaque, which may help to prevent heart disease.
- Low-density lipoprotein or LDL: This “bad” cholesterol circulates in your blood and, according to conventional thinking, may build up in your arteries, forming plaque that makes your arteries narrow and less flexible (a condition called atherosclerosis). If a clot forms in one of these narrowed arteries leading to your heart or brain, a heart attack or stroke may result.
Also making up your total cholesterol count are:
- Triglycerides: Elevated levels of this dangerous fat have been linked to heart disease and diabetes. Triglyceride levels are known to rise from eating too many grains and sugars, being physically inactive, smoking cigarettes, drinking alcohol excessively, and being overweight or obese.
- Lipoprotein (a) or Lp(a): Lp(a) is a substance that is made up of an LDL “bad cholesterol” part plus a protein (apoprotein a). Elevated Lp(a) levels are a very strong risk factor for heart disease. This has been well established, yet very few physicians check for it in their patients. (Lp(a) also was not assessed in the featured study.)
Study Finds Vitamin D + Calcium Supplementation Improves Lipid Profiles
The featured study sought to evaluate whether increased serum 25-hydroxyvitamin D3 (25OHD3) concentrations are associated with improved lipid profiles in postmenopausal women.
The study had over one million people so it was a big deal. The test group received a daily dose of 1,000 mg of elemental calcium along with 400 IUs of vitamin D3. Please note that this dose of vitamin D is ridiculously low and will not provide help for most people. The control group received a placebo.
Blood levels of vitamin D, fasting plasma triglycerides, HDL, and LDL cholesterol levels were assessed at the beginning and end of the trial. After two years, women who received the vitamin D and calcium supplements had a 38 percent increased mean vitamin D level compared to the placebo group.
They also had a 4.46-mg/dL mean decrease in LDL. Furthermore, higher vitamin D concentrations were associated with higher HDL combined with lower LDL and triglyceride levels. According to the authors:
”These results support the hypothesis that higher concentrations of 25OHD3, in response to [calcium/vitamin D3] supplementation, are associated with improved LDL cholesterol.”
After discussing the link between vitamin D and cholesterol with Dr. Seneff, I became convinced that raising your vitamin D levels through sun exposure may have far greater benefits than taking a supplement. I’ve even warned that vitamin D supplementation might not achieve optimal health results, the reason for which I’ll discuss in just a moment.
Remember that this study used a virtually insignificant dose of vitamin D that will not increase levels to optimum in anyone. Yet despite this nearly homeopathic dose, it still led to small, yet noticeable, improvements in lipid profile (i.e. increased HDL, in combination with reduced LDL and triglycerides).
Imagine what they would have found had they given doses 10 to 20 times higher that we know will put people into optimum ranges? In my view, this strengthens the hypothesis that naturally-acquired vitamin D, created by your skin in response to UV exposure, would likely have an even greater effect, and here’s why.
Cardiovascular Disease—A Compensatory Mechanism for Cholesterol Sulfate Deficiency?
Through her research, Dr. Seneff has developed a theory in which the mechanism we call “cardiovascular disease” (of which arterial plaque is a hallmark) is actually your body’s way to compensate for not having enough cholesterol sulfate. To understand how this works, you have to understand the interrelated workings of cholesterol, sulfur, and vitamin D from sun exposure.
Cholesterol sulfate is produced in large amounts in your skin when it is exposed to sunshine. When you are deficient in cholesterol sulfate from lack of sun exposure, your body employs another mechanism to increase it, as it is essential for optimal heart and brain function. It does this by taking damaged LDL and turning it into plaque.
Within the plaque, your blood platelets separate out the beneficial HDL cholesterol, and through a process involving homocysteine as a source of sulfate, the platelets go on to produce the cholesterol sulfate your heart and brain needs. However, this plaque also causes the unfortunate side effect of increasing your risk of cardiovascular disease. So how do you get out of this detrimental cycle?
Dr. Seneff believes that high serum cholesterol and low serum cholesterol sulfate go hand-in-hand, and that the ideal way to bring down your LDL (so-called “bad” cholesterol, which is associated with cardiovascular disease) is to get appropriate amounts of sunlight exposure on your skin. She explains:
“In this way, your skin will produce cholesterol sulfate, which will then flow freely through the blood—not packaged up inside LDL—and therefore your liver doesn’t have to make so much LDL. So the LDL goes down. In fact… there is a complete inverse relationship between sunlight and cardiovascular disease – the more sunlight, the less cardiovascular disease.”
What this also means is that when you artificially lower your cholesterol with a statin drug, which effectively reduces the bioavailability of cholesterol to that plaque but doesn’t address the root problem, your body is not able to create the cholesterol sulfate your heart needs anymore, and as a result you end up with acute heart failure.
Heart Disease Is the Number One Killer Worldwide
According to the World Health Organization (WHO), heart disease was the leading cause of death, globally, in 2011 and 2012. Even children are becoming increasingly at risk. Recent research suggests as many as one-third of children have or are at risk for high cholesterol, which conventional medicine views as a risk factor for heart disease.
Bear in mind that, contrary to the conventional ideology, your total cholesterol level—which includes HDL, LDL, triglycerides, and Lp(a)—is just about worthless in determining your risk for heart disease, unless it is above 300. Still, high total cholesterol can in some instances indicate a problem, provided it’s your LDL and triglycerides that are elevated and you have a low HDL. I have seen a number of people with total cholesterol levels over 250 who actually were at low heart disease risk due to their high HDL levels. Conversely, I have seen even more who had cholesterol levels under 200 that were at a very high risk of heart disease based on the following additional tests:
- HDL/Cholesterol ratio. This is a very potent heart disease risk factor. Just divide your HDL level by your cholesterol. That ratio should ideally be above 24 percent
- Triglyceride/HDL ratio. Here, you divide your triglyceride level by your HDL. This ratio should ideally be below 2
That said, these are still simply guidelines, and there’s a lot more that goes into your risk of heart disease than any one of these numbers. In fact, it was only after word got out that total cholesterol is a poor predictor of heart disease that HDL and LDL cholesterol were brought into the picture. They give you a closer idea of what’s going on, but they still do not show you everything. Additional risk factors for heart disease include:
- Your fasting insulin level: Any meal or snack high in carbohydrates like fructose and refined grains generates a rapid rise in blood glucose and then insulin to compensate for the rise in blood sugar. The insulin released from eating too many carbs promotes fat accumulation and makes it more difficult for your body to shed excess weight. Excess fat, particularly around your belly, is one of the major contributors to heart disease
- Your fasting blood sugar level: Studies have shown that people with a fasting blood sugar level of 100-125 mg/dl had a nearly 300 percent increase higher risk of having coronary heart disease than people with a level below 79 mg/dl
- Your iron level: Iron can be a very potent cause of oxidative stress, so if you have excess iron levelsyou can damage your blood vessels and increase your risk of heart disease. Ideally, you should monitor your ferritin levels and make sure they are not much above 80 ng/ml. The simplest way to lower them if they are elevated is to donate your blood. If that is not possible, you can have a therapeutic phlebotomy and that will effectively eliminate the excess iron from your body
Beware of Treating Elevated Cholesterol in Childhood with Drugs
Getting back to the study in question, a research team at Texas Children’s Hospital examined the medical records of more than 12,000 children between the ages of nine and 11, and found that 30 percent of them were at risk of elevated cholesterol levels. Elevated LDL and triglyceride levels were found to be more common among boys. Not surprisingly, obesity and lifestyle were deemed to be significant factors.
Universal cholesterol screening guidelines were issued in 2011, which strongly recommend all children be screened between the ages of nine and 11, and again between 17 and 21. The authors of the featured study say they hope their findings will give added weight to these guidelines. However, there are serious concerns that universal screening will simply place children on cholesterol-lowering medications, which do absolutely nothing to address the underlying problem… As reported by Eurekalert:
“‘There is concern by some in the medical community that children will be started on medication unnecessarily,’ [lead investigator, Dr. Thomas] Seery said, emphasizing that adopting a healthy diet and engaging in routine physical activity are first-line therapies for children with abnormal cholesterol levels.
He adds that cholesterol-lowering medications are typically needed in one to two percent of children with dyslipidemia, primarily in those with very high cholesterol resulting from a genetic lipoprotein disorder. Genetic lipoprotein disorders, such as familial hypercholesterolemia, result in very high cholesterol levels that can be detected in childhood but are felt to be underdiagnosed, he said. ‘Kids need to have their cholesterol panel checked at some point during this timeframe [9 to 11 years old],’ Seery said. ‘In doing so, it presents the perfect opportunity for clinicians and parents to discuss the importance of healthy lifestyle choices on cardiovascular health.’”
Read the Full Article Here.



 The FDA has NOT Banned Trans Fats! Traditional Saturated Fats like Coconut Oil Continue to Shine for Alzheimer's Disease but are Condemned by U.S. Dietary Advice
The FDA has NOT Banned Trans Fats! Traditional Saturated Fats like Coconut Oil Continue to Shine for Alzheimer's Disease but are Condemned by U.S. Dietary Advice The Evidence of Coconut Oil's Superiority Over Drugs in Destroying Pathogens Continues to be Published in Peer-Reviewed Journals
The Evidence of Coconut Oil's Superiority Over Drugs in Destroying Pathogens Continues to be Published in Peer-Reviewed Journals Study: Virgin Coconut Oil Protects Neuronal Damage and Mortality after a Stroke Incidence
Study: Virgin Coconut Oil Protects Neuronal Damage and Mortality after a Stroke Incidence Another Phase 3 Trial Failure to Develop an Alzheimer's Drug Shows Why Virgin Coconut Oil is Needed to Prevent Dementia
Another Phase 3 Trial Failure to Develop an Alzheimer's Drug Shows Why Virgin Coconut Oil is Needed to Prevent Dementia FDA Food Police want to Dictate What Foods are "Healthy" in New Guidelines Criminalizing Traditional Fats Like Butter and Coconut Oil
FDA Food Police want to Dictate What Foods are "Healthy" in New Guidelines Criminalizing Traditional Fats Like Butter and Coconut Oil